Title : Vitamin D Cuts SARS-CoV-2 Infection Rate by Half
link : Vitamin D Cuts SARS-CoV-2 Infection Rate by Half
Vitamin D Cuts SARS-CoV-2 Infection Rate by Half
Vitamin D Cuts SARS-CoV-2 Infection Rate by Half
- September 28, 2020
Story at-a-glance
- Based on data from 191,779 American patients, people with a vitamin D level of at least 55 ng/mL (138 nmol/L) had a 47% lower SARS-CoV-2 positivity rate compared to those with a level below 20 ng/mL (50 nmol/L)
- Based on data from 7,807 Israelis, those with a vitamin D level above 30 ng/mL (75 nmol/L) had a 58% to 59% lower risk of testing positive for SARS-CoV-2 compared to those with a vitamin D level below 29 ng/mL (74 nmol/L)
- Having a vitamin D level below 30 ng/mL also approximately doubles your risk of being hospitalized with COVID-19, Israeli researchers found
- Spanish researchers found giving hospitalized COVID-19 patients supplemental calcifediol (a vitamin D3 analog) in addition to standard of care lowered ICU admissions from 50% to 2% and eliminated deaths
- An August 2020 study found patients who had a vitamin D level below 12 ng/mL (30 nmol/L) had a 6.12 times higher risk of severe disease requiring invasive mechanical ventilation, and a 14.7 times higher risk of death compared to those with a vitamin D level above 12 ng/mL
Evidence showing vitamin D lowers your risk of SARS-CoV-2 infection, hospitalization, severe complications and death continues to mount. Most recently, a September 17, 2020, paper1 in PLOS ONE found people with lower vitamin D levels in their blood had a significantly higher risk of testing positive for SARS-CoV-2.
Higher Vitamin D Lowers Risk of Positive SARS-CoV-2 Test
The lead researcher in this study was Dr. Michael Hollick, who is widely recognized as one of the leading vitamin D experts in the world. I have interviewed him twice in the past. He and his team used retrospective observational analysis of SARS-CoV-2 tests to determine whether vitamin D blood levels impacted positivity rates.
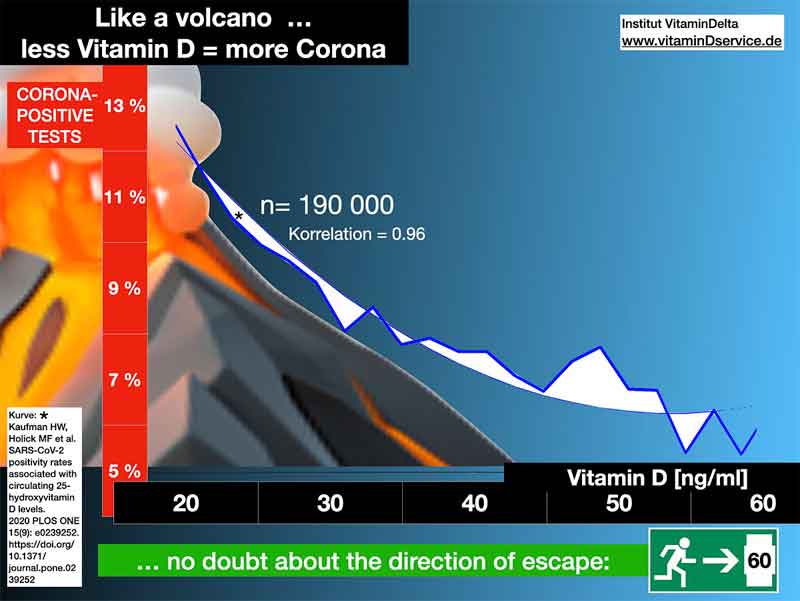
Based on vitamin D results from the preceding 12 months and SARS-CoV-2 test data from mid-March through mid-June 2020 from 191,779 patients from 50 U.S. states, people with a vitamin D level of at least 55 ng/mL (138 nmol/L) had a 47% lower SARS-CoV-2 positivity rate compared to those with a level below 20 ng/mL (50 nmol/L).2 As noted by the authors:
“The SARS-CoV-2 positivity rate was 9.3% and the mean seasonally adjusted 25(OH)D was 31.7 [ng/mL]. The SARS-CoV-2 positivity rate was higher in the 39,190 patients with ‘deficient’ 25(OH)D values (<20 ng/mL) (12.5% …) than in the 27,870 patients with ‘adequate’ values (30–34 ng/mL) (8.1% …) and the 12,321 patients with values ≥55 ng/mL (5.9% …) …3
The risk of SARS-CoV-2 positivity continued to decline until the serum levels reached 55 ng/mL. This finding is not surprising, given the established inverse relationship between risk of respiratory viral pathogens, including influenza, and 25(OH)D levels.4
SARS-CoV-2 positivity is strongly and inversely associated with circulating 25(OH)D levels, a relationship that persists across latitudes, races/ethnicities, both sexes, and age ranges. Our findings provide impetus to explore the role of vitamin D supplementation in reducing the risk for SARS-CoV-2 infection and COVID-19 disease.”5
The graph below, obtained from GrassrootsHealth,6 shows how the rate of positive SARS-CoV-2 results declines as vitamin D levels go up. Again, as you increase your vitamin D level from 20 ng/mL to 55 ng/mL, your risk of having a positive SARS-CoV-2 test result decreases by 47%.
Even after adjustment for gender, age, ethnicity and latitude, the risk of having a positive test result was 43% lower among those with a vitamin D level of 55 ng/mL compared to those with a level of 20 ng/mL. I understand that the COVID-19 test may be worthless and counterproductive with its false positives, but it is the only metric we currently have to assess interventions.
Vitamin D Lowers Infection and Hospitalization Rates
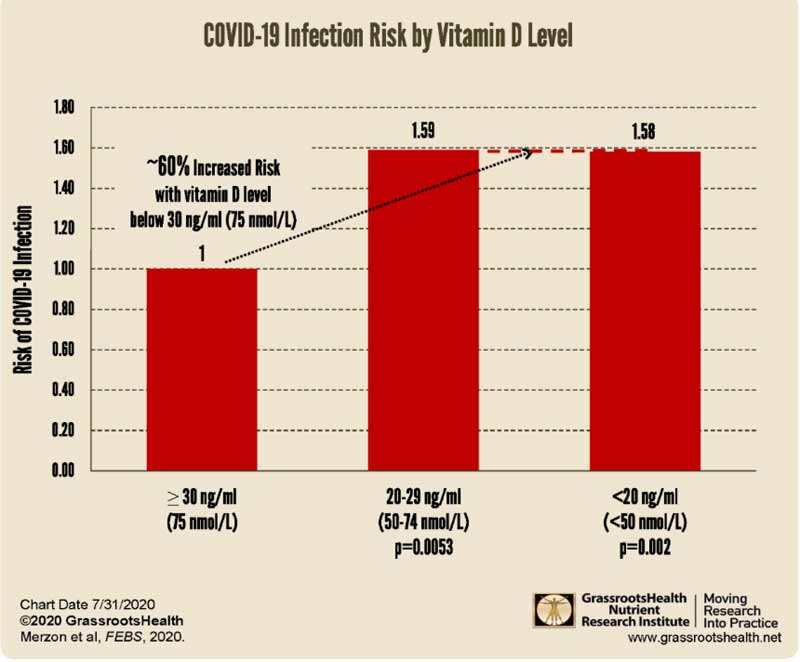
That higher vitamin D levels lower the risk of SARS-CoV-2 infection (i.e., getting a positive test result) was also confirmed in an Israeli population-based study7,8 published in July 2020. This paper examined data from 7,807people tested for SARS-CoV-2 infection between February 1 and April 30 of 2020 who also had vitamin D test data available.
Here, those with a vitamin D level above 30 ng/mL (75 nmol/L) had a 59% lower risk of testing positive for SARS-CoV-2 compared to those with a vitamin D level between 20 ng/mL and 29 ng/mL (50 to 74 nmol/L), and a 58% lower risk compared to those with a vitamin D level below 20 ng/mL (50 nmol/L). The graph below, from a GrassrootsHealth report,9 illustrates the findings.
Vitamin D Lowers Hospital and ICU Admissions
Seeing how higher vitamin D levels lowers your risk of testing positive for SARS-CoV-2 in the first place, it’s no surprise then that other data show higher vitamin D also lowers hospital and intensive care admissions.
The Israeli analysis10 above, for example, found that among individuals who tested positive for SARS-CoV-2 infection, those who had a vitamin D level below 30 ng/mL also had a 1.95 times (crude odds ratio) to 2.09 times (odds ratio after adjustment for demographics and psychiatric and somatic disorders) higher risk of being hospitalized for COVID-19.
In other words, having a vitamin D level below 30 ng/mL about doubled the risk of being hospitalized with COVID-19. Vitamin D, when administered to hospitalized patients, can also lower their risk of needing intensive care.
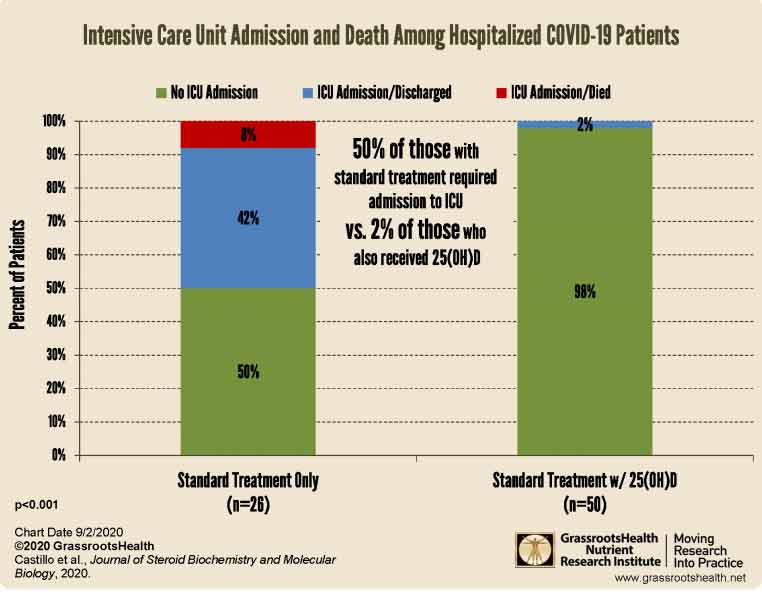
This was demonstrated by Spanish researchers in a small randomized clinical study11,12,13,14 published online August 29, 2020. They found hospitalized COVID-19 patients who were given supplemental calcifediol (a vitamin D3 analog also known as 25-hydroxycholecalciferol or 25-hydroxyvitamin D) in addition to standard of care — which included the use of hydroxychloroquine and azithromycin — had significantly lower intensive care unit admissions.
Patients in the vitamin D arm received 532 micrograms of calcifediol on the day of admission (equivalent to 106,400 IUs of vitamin D15) followed by 266 mcg on Days 3 and 7 (equivalent to 53,200 IUs16). After that, they received 266 mcg once a week until discharge, ICU admission or death.
Of those receiving calcifediol, only 2% required ICU admission, compared to 50% of those who did not get calcifediol. None of those given vitamin D supplementation died, whereas 7.6% in the standard care group perished.
Vitamin D Lowers COVID-19 Mortality
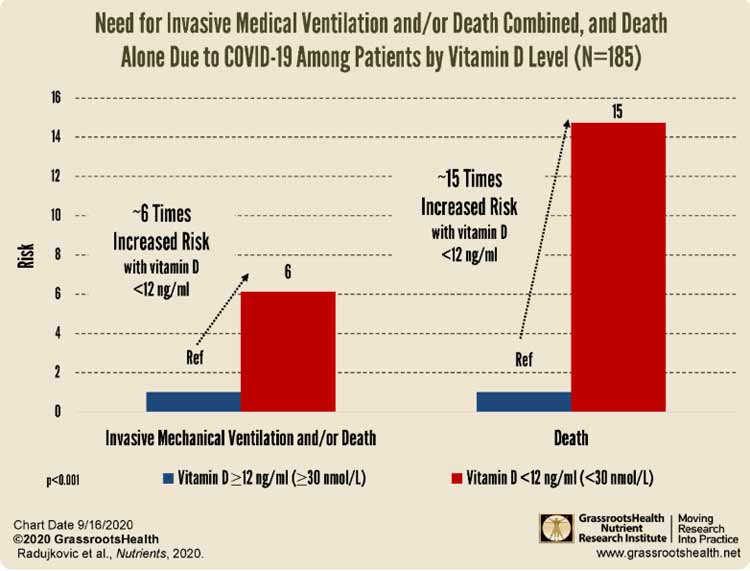
Other studies have also confirmed that higher vitamin D levels lowers your risk of complications and death from COVID-19. Among them is an August 2020 study17,18 published in the journal Nutrients, which found patients who had a vitamin D level below 12 ng/mL (30 nmol/L) had a 6.12 times higher risk of severe disease requiring invasive mechanical ventilation, and a 14.7 times higher risk of death compared to those with a vitamin D level above 12 ng/mL.
An Iranian study19,20 published online in mid-July 2020 also found that patients with vitamin D levels above 30 ng/mL (75 nmol/L) had better clinical outcomes and a far lower risk of death. Among COVID-19 patients over the age of 40 who had vitamin D levels below 30 ng/mL, 20% died, compared to 9.7% of those with levels at or above 30 ng/mL. Among those with a vitamin D level of at least 40 ng/mL, only 6.3% died.
Low Vitamin D Is a Risk Factor for Respiratory Failure
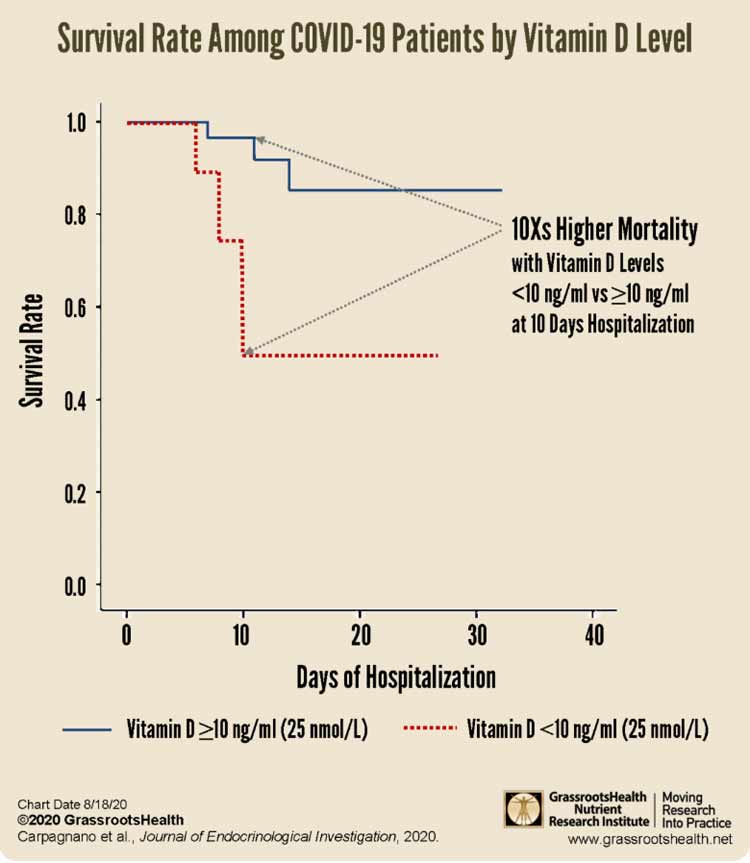
Yet another study, published in the Journal of Endocrinological Investigation in August 2020, found vitamin D deficiency was a common factor among hospitalized patients in Italy who had been diagnosed with COVID-19 related respiratory failure.
As reported by GrassrootsHealth:21
“Vitamin D levels were measured for each patient and were defined as insufficient (20-29 ng/ml or 50-74 nmol/L), moderately deficient (10-19 ng/ml (25-49 nmol/L), and severely deficient (<10 ng/ml or <25 nmol/L). A normal vitamin D level was defined as 30 ng/ml (75 nmol/L) or higher.
81% of the patients with acute respiratory failure due to COVID-19 had vitamin D levels below 30 ng/ml (75 nmol/L); and 24% had severe vitamin D deficiency (≤10 ng/ml or ≤25 nmol/L).
When looking at mortality rates after 10 days of hospitalization, it was found that those with severe vitamin D deficiency had a 50% probability of death, compared to 5% among those with a vitamin D level greater than 10 ng/ml (25 nmol/L).
This is a 10 times higher risk of death among patients with severe vitamin D deficiency compared to patients with vitamin D levels >10 ng/ml (>25 nmol/L) at 10 days of hospitalization."
According to the study authors:
“Altogether, these considerations support the recommendation that people at risk of influenza and/or COVID-19 consider vitamin D supplementation to raise their 25(OH)D concentrations above 40-60 ng/mL, and that treatment of patients infected with influenza and/or COVID-19 includes higher vitamin D doses.”
How and Why Vitamin D Lowers COVID-19 Risks
In “Bradykinin Hypothesis Explains COVID-19 Complexities,” I reviewed how vitamin D lowers your risk of COVID-19 complications and death by inhibiting both cytokine22 and bradykinin storms.23 Vitamin D also:
|
Lowers viral replication24 |
|
Boosts your overall immune function by modulating both innate and adaptive immune responses |
|
Reduces respiratory distress25 |
|
Improves overall lung function |
|
Helps produce surfactants in your lungs that aid in fluid clearance26 |
|
Lowers your risk of comorbidities associated with poor COVID-19 prognosis, including obesity,27 Type 2 diabetes,28 high blood pressure29 and heart disease30 |
All of these factors make it an important component of COVID-19 prevention and treatment. As temperatures and humidity levels drop — two factors that influence the viability of SARS-CoV-2 in air and on surfaces — it’s quite likely we’ll see a reemergence as we move into fall and winter.
My #StopCOVIDCold campaign seeks to raise awareness about the importance of vitamin D optimization to prevent a resurgence of COVID-19 hospitalizations and deaths. The two reports, which you can download free of charge on the #StopCOVIDCold website, provide in-depth information about the biological mechanics behind vitamin D’s protective effects.
Now, as the northern hemisphere heads into autumn, is the ideal time to check your vitamin D level and start taking action to raise it if you’re below 40 ng/mL (100 nmol/L). Experts recommend a vitamin D level between 40 and 60 ng/ml (100 to 150 nmol/L). An easy and cost-effective way of measuring your vitamin D level is to order GrassrootsHealth’s vitamin D testing kit.
Once you know your current vitamin D level, use the GrassrootsHealth vitamin D calculator31 to determine how much vitamin D you might need to reach your target level.
To optimize vitamin D absorption and utilization, be sure to take your vitamin D with vitamin K2 and magnesium. As explained in “Magnesium and K2 Optimize Your Vitamin D Supplementation,” taking magnesium and vitamin K2 can lower your oral vitamin D requirement by as much as 244%.
Lastly, remember to retest in three to four months to make sure you’ve reached your target level. If you have, then you know you’re taking the correct dosage. If you’re still low (or have reached a level above 80 ng/mL), you’ll need to adjust your dosage accordingly and retest again in another three to four months.
Thus Article Vitamin D Cuts SARS-CoV-2 Infection Rate by Half
You are now reading the article Vitamin D Cuts SARS-CoV-2 Infection Rate by Half with the link address https://polennews.blogspot.com/2020/09/vitamin-d-cuts-sars-cov-2-infection.html

0 Response to "Vitamin D Cuts SARS-CoV-2 Infection Rate by Half"
Post a Comment